Whether You Decide to Work With Us or Not, Let Us Explain Just A Few Things To Help You Make A Confident Decision
You may have said or thought these types of things:
- “I would prefer to use my insurance benefits for PT.”
- “That seems like a lot of money.”
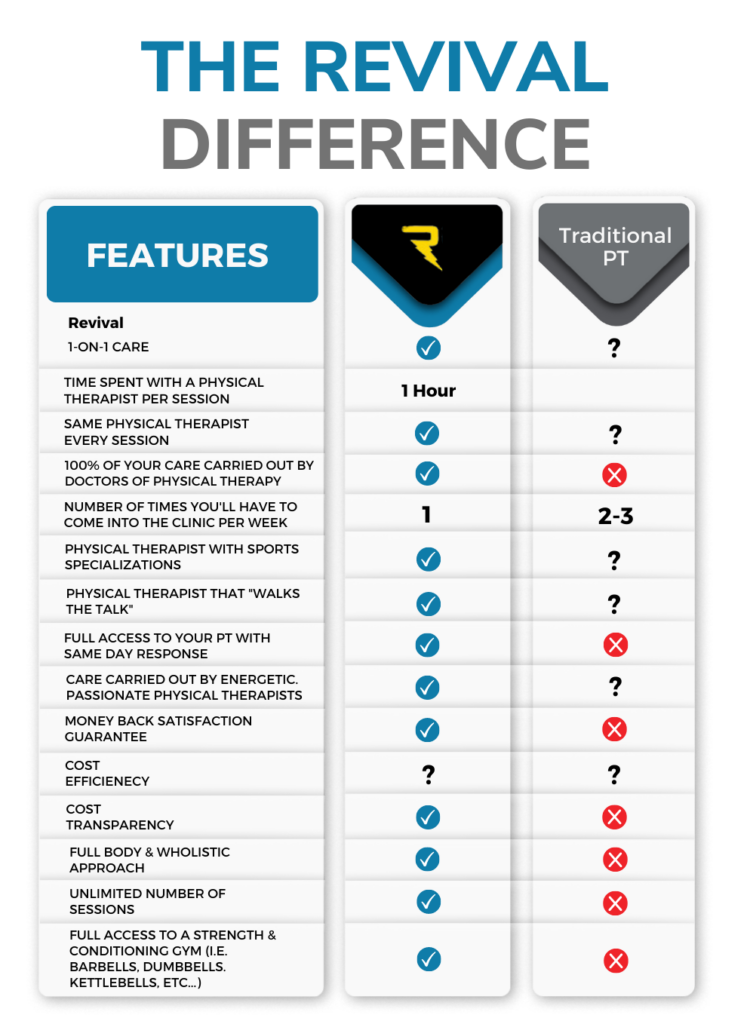
It’s totally normal for you to feel this way. The current healthcare landscape for active-adults and athletes is changing drastically. As insurance companies continue to reduce payment to PTs the quality of care that patients are receiving is being reduced. Co-pays are also at all-time highs and continue to increase. Below is some insight into how working with an out-of-network practice like Revival Physical Therapy and Wellness can actually save you not only money, but time as well and ultimately lead to better results than a traditional, in-network practice.
Whether You Decide to Work With Us or Not, Let Us Explain Just A Few Things To Help You Make A Confident Decision
The short answer:
In many ways, insurance companies dictate or strongly influence the treatment that patients receive at “in-network” clinics, and we refuse to allow that to be the case at Revival Physical Therapy and Wellness.
The longer answer:
We are an out-of-network practice because the business model necessary for an in-network practice to survive rarely ever allows for the high-level care we insist on giving our patients.
What the heck does that mean? …
Due to progressively worsening reimbursement rates and pressure from insurance companies, the therapists at in-network clinics have to see at least 2 patients per hour (usually many more) and they often use technicians and assistants to provide much of the actual patient care. The care often includes modalities like heat packs and ultrasound, and the majority of a patient’s time at the clinic is spent doing exercises they could do on their own time. Furthermore, these types of clinics tend to require patients to attend 2-3 appointments per week.
We do not believe that modalities are nearly as effective as our hands-on treatment, and we also do not agree with having patients pay to perform exercises in the clinic that they can easily perform at home or at a gym. All of our patients receive one-on-one care and hands-on treatment from a Doctor of Physical Therapy in every session. With this one hour long-session, one-on-one treatment approach, the plan of care for the vast majority of our patients only involves one appointment per week.
When you consider the time savings of fewer trips to the clinic and the value of resolving your pain so much faster than average, the out-of-pocket expense at Revival Physical Therapy and Wellness is a huge bargain.
On top of that, the out-of-pocket expense for our treatment sessions is sometimes less than a patient would pay at a clinic that accepts and bills their insurance.
How is that possible?!
As deductibles and PT copays have skyrocketed in recent years, many of our patients who have high PT copays or have not met their deductible pay less out of pocket for our treatments than they would if they went to a clinic that “takes their insurance.”
So before deciding on where to get PT based solely on which clinics “take your insurance,” make sure you know how much you’ll be paying at your in-network options versus an out-of-network clinic like ours …
These days, some insurance plans provide zero coverage for PT visits or require copays of over $50/visit. And if you have a deductible to meet, you’ll likely end up paying the full bill for your PT sessions until you meet the deductible (and these bills are often $200+ per session). However, you usually won’t start receiving those $200+ bills until after you’ve been getting care for 6-8 weeks and have racked up an enormous total balance (again, often being asked to attend PT 2-3 times per week).
And guess what else… just because you’re paying $200+ per session at a clinic that is in-network with your insurance, does not mean that your insurance is applying that full amount towards your deductible! They often only apply the amount that they have agreed is reasonable for your PT sessions which is, of course, far less than the amount the PT clinic actually charges.
Most people are quite unaware of the games their insurance companies play in order to pay out as little as possible and maximize their profits.
To help level the playing field, we’ve provided you with a list of questions to call and ask your insurance about to help you get the full picture:
1. “What percentage of the total PT bill will I be required to pay at an in-network clinic?”
This question is especially important if you still have a deductible to meet. If you will be paying 100% of the bill until you’ve met your deductible, ask the prospective PT clinic the amount of the average bill sent to an insurance company. In most cases, you will ultimately be paying the full bill until your deductible is met.
2. If you have met your deductible, ask: “How much will my copays be for each visit?”
Consider the quality of care you’ll be receiving at your various options, and how much value you place on receiving higher-quality, one-on-one care from a Doctor of Physical Therapy rather than a PT Assistant (PTA) or an unskilled “Tech.”
Consider how often you’ll be missing work and/or time with family to attend your PT sessions. Again, you can ask any prospective clinic how many times per week their average patient is asked to come in for treatment.
Ask the above questions, do the math, and you may be quite surprised at what you find!
With all the above information, you can now get a real sense of what your true costs will be, what level of care you’ll be getting, and then make the best decision on where to receive your physical therapy treatment.
Can I bill my insurance for reimbursement of my out-of-pocket expenses?
This depends on the insurance you have, but YES, most NON-Medicare patients can send “self-claims” to their insurance company for their treatments at our clinic. You should be able to submit through your insurance company’s online portal. We provide all of our patients with the needed receipts and treatment codes that they need to do so.
The amount of reimbursement or application towards your deductible is completely dependent on your insurance plan. If you call your insurance company to inquire about what you can expect to receive, you should ask about reimbursement for “out-of-network Physical Therapy” expenses sent in via self-claims.
“I Still Want to Call Around to Find a Place That Takes My Insurance”
This can be a totally sensible thing to think about and want to do. We’ve included a checklist below of questions that will help you get the full picture of the quality of care you can expect to receive from each option.
WHAT TO ASK A PHYSICAL THERAPY CLINIC
- How much 1-on-1 time will I get with the doctor of physical therapy each visit?
- Will I have the same PT every session?
- How many visits per week are typically prescribed?
- How long is the average plan of care?
- Do your PTs specialize in the services I need?
- Can you guarantee that I will never get a surprise bill?
- What is the amount of the average bill you will be sending to my insurance company?
- With all the above information, you can now get a real sense of what your true costs will be, what level of care you’ll be getting, and then make the best decision on where to receive your physical therapy treatment.
